Highmark Health is piloting a new program that addresses food insecurity and will provide eligible members with medically-tailored meals, the company announced Monday.
The six-month pilot program aims to support 1,000 Highmark insurance members with certain chronic health conditions and who are at high-risk of food insecurity. Eligible chronic conditions include chronic kidney disease, congestive heart failure, hypertension and diabetes. These members will receive two medically-tailored meals a day, as well as coaching and social work to help them live a healthier lifestyle.
In addition to addressing food insecurity, Highmark’s program will work to reduce other areas of health inequity as well, said Nebeyou Abebe, senior vice president of social determinants of health at the company.
“When we engage the member and realize that they’re food insecure, we’re also assessing for other health-related social needs,” Abebe said in an interview. “This person could have transportation issues or be dealing with housing issues or domestic violence. That presents another opportunity for our social worker to have a conversation with a member.”
As the program goes on, Highmark will track members’ level of engagement, as well as clinical measurements like blood sugar and emergency room visits. Tracy Saula, senior vice president of product and health experience at Highmark Health, hopes the program will not only improve members’ health, but lower healthcare costs as well.
“We believe that it could easily result in obviously improved health, which is the most important,” Saula said in an interview. “But also a reduction in total cost of care, somewhere between 10-16% … Our goal in this is to identify, is this the kind of benefit we could provide longer term?”
There is a strong link between nutrition and health, research shows. People who are food insecure have a higher risk of chronic diseases, increased hospitalizations, higher cost of care and mental health challenges, according to the Robert Wood Johnson Foundation. Additionally, a recent study published in JAMA Network Open found that if payers provided medically-tailored meals to patients with diet-sensitive limitations, they could save $13.6 billion annually.
The food as medicine movement has gained momentum recently, particularly after the White House held a conference in September about food insecurity. Abebe said Highmark’s new program is in alignment with the White House’s efforts. Other healthcare organizations addressing food insecurity and nutrition include Kaiser Permanente and Geisinger.
Saula said she hopes Highmark’s initiatives can ultimately prove the benefit of programs that address food insecurity so that more healthcare players get involved.
“If you want to start to truly think about food as medicine and treat it as such — which means insurers paying for it the same way an insurer would pay for a diabetic medicine — they need proof that it works,” Saula said.
Photo: vgajic, Getty Images
Uncategorized
WebMD Provider Services on Wednesday struck a partnership with patient communication company Artera (formerly WELL Health) to expand access to patient educational content and medication affordability programs.
WebMD Provider Services is a division of healthcare news publisher WebMD. The division provides patient education and engagement solutions for hospitals, health systems and other providers, said Ann Bilyew, senior vice president of WebMD Provider Services, in an interview.
Artera sells its patient communication software to hospitals, health systems and large physician networks. The company delivers “the technology that allows facilities to engage with their patients outside of the point of care in a streamlined, unified manner,” said Guillaume de Zwirek, Artera’s founder and CEO. Most of Artera’s patient communication strategy centers on text messages, so it doesn’t compete with patient portals, de Zwirek pointed out. He said his company is more focused on the last mile.
WebMD decided to partner with Artera because it believes the company can help it deploy its vast amount of content and information more efficiently, Bilyew said. WebMD has a trove of information that patients can use to make better decisions and advocate for themselves during their care journey, but it’s critical that this information reaches patients conveniently and at the right time, she pointed out.
“Partnering with a company like Artera enables us to put our content in the hands of patients, when it’s most convenient for them,” Bilyew declared. “And certainly a lot of our health system customers already use Artera. So it’s easy for us to help them leverage the investment they’re already making in Artera and the investment that they’re making in our patient education. We put those two things together to help them get the most out of it.”
Under this collaboration, patients will receive messages from their providers and they will have the ability to respond back. Sometimes the responses will be automated, and sometimes a person will write them, de Zwirek said.
For example, if a patient is discharged from the hospital after a hip replacement, they could receive a text with physical therapy exercises to help them recover. Let’s say they received a list of exercises for their right hip, but it was the left one that they got replaced. The patient is able to respond to the text and ask for left hip exercises, and a member of the provider’s staff will quickly correct that error, according to de Zwirek.
And let’s say this patient realizes they won’t be able to make an upcoming physical therapy appointment. Under this collaboration, they can text their provider and a cancellation or rescheduling request automatically gets fulfilled because Artera is integrated with the EHR.
The partnership deploys text messages because SMS is a channel proven to produce high engagement levels, de Zwirek said.
In fact, Artera conducted a study recently with a large hospital customer. It looked at 94,000 patients. For half of them, Artera honored patient preferences in the EHR, meaning it did not text them if they had opted out of text messaging. For the other half, the company ignored the patient preferences and texted anyway. The results showed that the vast majority of patients with “no texting” preferences in the EHR did not actually opt out once they received a text from their provider.
Both de Zwirek and Bilyew said they would like to get their joint customers on board with this partnership as soon as possible.
“I think it’s going to make such a difference for providers’ ability to continue a relationship with a patient. And it’s going to make such a difference for the patient in terms of giving them access to quality information and helping them stay adherent to the care plans that their providers and physicians put together for them,” Bilyew said.
Photo: Vladyslav Bobuskyi, Getty Images
Ekso Bionics — a San Rafael, California-based company that makes exoskeleton bionic devices — on Monday acquired Parker Hannifin’s business unit for human motion and control for $10 million. Parker is an Ohio-based manufacturer specializing in motion and control technologies. It received $5 million from Ekso at the deal’s closing, and it will receive the remaining $5 million over the next five years.
The acquisition will help extend Ekso’s product line across the continuum of care and provides access to Vanderbilt University as a research partner, said Ekso CEO Scott Davis in an interview.
Born out of University of California Berkeley’s robotics program, Ekso became a company in 2005. Seven years later, it launched its first commercial medical rehabilitation exoskeleton.
Since then, the company has received 510(k) clearance from the FDA to market its EksoNR robotic exoskeleton for use by people with spinal cord injury, traumatic brain injury, stroke and multiple sclerosis. The robotic device is designed for use in rehabilitation settings and is meant to help neurorehabilitation patients learn how to walk properly again.
With the acquisition, Ekso is gaining Parker’s Indego lower limb exoskeleton line of products that allow clinicians to deliver individualized gait therapy to patients in inpatient, outpatient and home settings. The purchase also brings Parker’s robotic-assisted orthotic and prosthetic devices, which are currently being developed with hopes of commercialization in the future. The Indego product line allows clinicians to deliver individualized gait therapy to patients in inpatient, outpatient and home settings.
The MS indication for EksoNR increased Ekso’s capabilities in the outpatient space, but the acquisition of the Indego product line brings the company further into the outpatient setting and into the home, Davis pointed out.
“There’s something that happens among patients who have been using our technology and making great strides in their recovery through the use of robotic therapies. As they progress and as they move from inpatient to outpatient, they are often brought into more traditional physical therapy methods. And when they go home, oftentimes they’re left with no exoskeleton or augmented therapies. So this acquisition allows us to sort of follow that patient from post-acute care into outpatient and into the home,” he said.
The transaction also brings Parker’s 10-year research and development partnership with Vanderbilt University to Ekso. Davis said he expects Ekso and Vanderbilt to work together to create more innovative products in the future.
Ekso had been looking for a strategic acquisition to extend its products across the continuum of care for “a long time,” Davis declared.
“We’ve looked at every company that you can imagine in this space,” he said. “The synergies were so obvious between the organizations from the very first meeting that the time had to be now.”
Photo: Natee Meepian, Getty Images
If the Covid-19 public health emergency expires in April, about 18 million people could lose Medicaid coverage, a new report concludes.
The Urban Institute, which published the report, found that of these 18 million people, 3.8 million people will become completely uninsured. About 3.2 million children will likely move from Medicaid to separate Children’s Health Insurance Programs. Additionally, about 9.5 million people will receive employer-sponsored insurance. Lastly, more than 1 million people will enroll in a plan through the nongroup market.
The Urban Institute’s estimates, published Monday, is higher than the U.S. Department of Health & Human Services’ (HHS) prediction of 15 million people losing coverage after the public health emergency ends. HHS’ report was published in August and stated that 17.4% of Medicaid and Children’s Health Insurance Program enrollees would leave the program. The Urban Institute’s report did not provide a percentage.
T0 conduct the study, researchers from the Urban Institute relied on the most recent administrative data on Medicaid enrollment, as well as recent household survey data on health coverage. It used a simulation model to estimate how many Americans will lose Medicaid insurance.
In 2020, Congress passed the Families First Coronavirus Response Act due to the Covid-19 pandemic. It barred states from disenrolling people during the public health emergency, and in return, states received a temporary increase in the federal Medicaid match rates. From February 2020 to June 2022, Medicaid enrollment increased by 18 million people, an unprecedented number, according to the Urban Institute.
Currently, the public health emergency is set to end in January. But since the government has to provide a 60-day notice before the expiration —and did not do so in November — it is expected to be extended to April.
Because many of the affected enrollees who will lose Medicaid coverage will be eligible for coverage through federal or state Marketplaces, the Urban Institute recommends coordination between the Marketplaces and state Medicaid agencies
Researchers called on the government to take action so Americans are prepared for the end of the public health emergency.
“State Medicaid officials and policymakers must continue to ensure that individuals currently enrolled in Medicaid are aware of the approaching end of the public health emergency, and that they have a plan to maintain or find new health coverage through their employer, the federal healthcare Marketplace, or Medicaid,” the Urban Institute said.
Photo: designer491, Getty Images
Every organization talks about innovation, but all too often they view it as something external — a new technology to adopt or a device to purchase. Rather than foster an internal culture of innovation, they watch for others to emerge in their industries and go no further than a build-vs-buy evaluation of something already created by someone else.
In healthcare, a lack of innovation culture can lead to suboptimal patient outcomes. Lives and futures depend on systems, processes, and clinicians’ skills and actions. We must constantly update the ways we provide care to meet a fast-changing world whose rate of change will only increase. The most effective innovations bubble up from practical needs recognized and developed by frontline care teams in the real world. Over my 15+ years of ongoing work on the front lines of emergency medicine I have seen this firsthand.
Healthcare organizations are largely made up of people who pour their hearts and souls into working long hours trying to bring better health to as many people as they can. But typically at the organizational level, these frontline folks’ passion, dedication, and practical solutions are not captured, leveraged, and widely shared.
Here are three foundational approaches healthcare leaders can use to let the experience and insights of care teams fuel innovations that the organization can develop and bring to the world. The challenge is that each approach may run counter to company culture. The organization must actively choose, plan, and act to create a place inside its walls where innovation isn’t a buzzword but part of the core mission.
Tie innovators to real-world needs, not revenueTrying new ways to improve outcomes is part of a big-picture business strategy, but it isn’t always a new product line. It’s too common for innovators to be challenged from the start to justify their own jobs by reporting ROI on their projects, as if they were the business development team. Impatient executives may see innovators’ exploration as wasting time, burning cash, or ivory-tower pontificating.
I’m not suggesting that self-styled innovators do whatever they want. Rather, keep them connected with and listening to care teams in the real-world. What frustrates physicians trying to diagnose and treat patients today? How would nurses be able to spend more time on care, or just less on repetitive data entry? Are there new applications of machine learning and other technologies that would actually improve outcomes? These are front-line challenges where advanced expertise could find the most optimal ways to apply emerging technologies and approaches. Step back from insisting everything be proven profitable before it’s even developed.
Accept some failures as part of successLarge companies tend to attract professionals whose top skill may be not getting fired. They’ll never make a big mistake, because they’ll never take a big risk. They’re great at identifying problems, but not at proposing solutions that could fail. They know that if the entire organization fails in the long term, no one will blame them personally — hey, they worked hard to turn things around! On to the next role at the next company.
It needs to be OK to take big risks, as failures are necessary steps in the path to future success. Any parent knows children learn to walk by falling down a lot. Of course, people tasked with innovations should be evaluated on their work, but the success or failure of the would-be innovation shouldn’t be the sole metric of their personal performance.
Rather, they should know it’s on them to do everything they can to navigate their bright idea all the way to clinical practice, and keep the organization informed of unexpected setbacks or unforeseen obstacles that prove impassable. Accepting the right failures is wise for the organization, because often those who have failed before are now the best qualified to succeed this time.
Look outside, then grow withinOrganizations often do look at what others are doing, but only in a “should we get that, too” way. Build-vs-buy projects too often pass for innovation when they’re more like shopping. Beyond evaluating what to adopt that others have, look at how an innovation elsewhere can be applied in a parallel but different way to the challenges your organization seeks to conquer. Squelch the organization’s natural tendency toward “not invented here” dismissal of ideas from outside. Reward curiosity and research instead.
Explore other industries and look for parallel benefits you could bring to yours. See how food delivery has removed the phone tag and clumsy online forms that still hobble patients trying to schedule with physicians and clinics. Find out how banks digitized and automated financial transactions in ways that would literally change the economics of medical claims processing. You might even find a way to work with other companies to co-develop a new approach.
Fostering innovation at large organizations is a challenge. Just talking about how to do it is an industry in itself. For many, though, the place to start is to create a space and a structure inside the organization where it can happen. Connect innovators to real-word care teams. Give innovators guidelines that reward hard-fought failures. Look outside your organization and industry for breakthroughs to adapt, rather than products or procedures to adopt. Innovation isn’t something you acquire. It’s something you grow from within.
Photo: ipopba, Getty Images
The worst of Covid-19 may be behind us, but the pandemic continues to have a negative impact on margins and healthcare revenue with 2022 poised to be the worst financial year since the beginning of the pandemic. Costs for everything are up, inflation is at around 7.7% and all health systems are facing staffing shortages in both clinical and administrative positions. A recent study indicates that 92% of revenue cycle teams are understaffed with 1/3 understaffed by more than 20 positions.
The healthcare worker shortage has deeply impacted revenue cycle operations. Kaufman Hall survey respondents cited increased rates of claims denials (67%), a lower percentage of commercially insured patients (51%), and an increase in bad debt/uncompensated care (41%).
Given these alarming numbers, it’s no surprise that nearly half (46%) of U.S. hospital and health system finance leaders responding to another survey said their organizations currently are behind their 2022 revenue goals.
The labor shortage is here to stay. Staffing experts indicate that the shortage will remain for at least five years, leaving chief financial officers and rev cycle vice presidents struggling to fill positions left vacant by overworked, burned-out employees who quit over the past two strenuous years. When 30% to 40% of receivables aren’t being worked because of staffing shortages in the revenue cycle, it leads to lower collections, payment delays or less cash on hand that can devastate a hospital or health system’s finances.
Increased competition for patients from Walgreens, CVS and other disruptors are further squeezing margins for hospitals and health systems. Healthcare labor costs have skyrocketed because of overtime pay and travel nurses, both of which can add roughly 50% to a typical employee’s hourly rate.
Consultants will tell you that any problem can be solved through people, process and technology. Well, hospitals don’t have enough people, while processes in healthcare are largely antiquated and sometimes broken. That leaves technology as the best strategy for success.
An automation strategy
The good news is that hospitals and health systems are embracing automation as a solution to their operational challenges, particularly in the revenue cycle. Much of the work in the revenue cycle involves critical but redundant tasks.
Automation enables digital workers or ‘bots’ to do many of those repetitive tasks. A revenue cycle worker can handle about 400 accounts a week, whereas a bot can process about 4,750 accounts weekly at an average cost of $2.40 per account. That’s an 1,100% increase in efficiency combined with a 75% reduction in cost. By leaning into automation, revenue cycle leaders can attain the operational efficiencies they need to optimize revenue while saving money.
Here are three quick tips for hospitals and health systems to successfully implement automation technology in their revenue departments:
Automate with intentSure, when you have an automation hammer, everything looks like a nail. But your strategy shouldn’t be to automate everything. (In fact, that’s not even a strategy!)
Rather, you should pursue a data-driven approach that starts by identifying your biggest pain points. Look at the data to determine which processes bots can perform to ease those pain points. Let’s say the data shows that human errors are contributing to an unacceptably low “clean claim rate” (the metric for quality of claims data). If bots can be used to autofill information without mistakes, errors will be reduced and the claims process accelerated, meaning faster time to payment.
Experiment and learn incrementallyOnce you’ve developed an automation strategy that identifies areas of priority, begin implementation on a small scale to ensure there are no unanticipated problems.
Start by automating the most mechanical tasks in the revenue cycle. Measure results and make necessary changes. Build upon your successes and gradually progress to jobs that require artificial intelligence (AI)-driven insights and analytical work to uncover patterns and detect anomalies such as coding errors.
Continue to build your automation platform incrementally, drawing on your data feedback loop to fine-tune performance.
Have a plan for rev cycle staffAutomating billing and claims tasks can ease the pressure on chronically understaffed rev cycle departments. It also presents an opportunity to free up rev cycle employees from mundane and time-consuming administrative tasks, allowing them to focus on higher-value activities that directly drive revenue. Prior authorization is a great example for automation. A recent American Medical Association report indicates that practices are spending an average of 16 hours per week on prior authorization submission. Automating that process for your major payers is a critical timesaver.
Outsourcing low value but essential tasks to bots can improve operational efficiency and save money by reducing the need to pay overtime or hire expensive contract workers. Automation also can reduce employee satisfaction because rev cycle workers feel that their jobs are meaningful to the organization.
Hospitals and health systems must take advantage of the opportunity automation provides them by developing a human redeployment strategy for upskilling rev cycle staff to perform tasks that involve critical thinking and judgment.
Conclusion
Hospital and health system revenue cycles will face a labor shortage and external economic pressures for the indefinite future. Automation can help streamline and optimize healthcare revenue cycles, but organizations must use this enabling technology with strategic intent.
Photo: Andranik Hakobyan, Getty Images
Intermittent fasting is all the rage today as people follow this method to gain health benefits. But a new study suggests that there may be possible negative consequences of fasting intermittently.The study, published in the journal Eating Behaviors, found intermittent fasting in adolescents and younger population can lead to behaviors and psychopathology of eating disorders and other dangerous behaviors.There are different ways of intermittent fasting. One is to fast on two non-consecutive days of the week. Another is to fast for certain periods of time. An example of this type of intermittent fasting is the 16/8 method, which involves fasting for 16 hours and eating only in an 8-hour window.“With proper guidance from a registered dietitian, a client can be guided into choosing well-balanced foods within the method of 16:8; I like this method because it’s basically eating three meals within a workday. A chronic dieter may skip meals or avoid many good foods,” Blanca Garcia, RDN, a Los Angeles-based registered dietitian nutritionist and nutrition specialist with the Measurement Instrument Database for Social Sciences (MIDSS), not involved in the study, told Medical News Today.
Some evidence suggests intermittent fasting aids in weight loss. But the technique has its pitfalls.The researchers found a relationship between intermittent fasting and eating disorders among adolescents and young adults.For the study, researchers used data from the Canadian Study of Adolescent Health Behaviors. The study included 2,762 adolescents and young adults, including women, men, and transgender or gender non-conforming individuals, according to the outlet.“IF [Intermittent fasting] was highly common among the sample, including 48% of women, 38% of men, and 52% of transgender/gender non-conforming participants, and participants fasted for, on average, 100 days in the past 12 months,” Study author Kyle T. Ganson, assistant professor and Factor-Inwentash Faculty of Social Work with the University of Toronto, Canada, said, the outlet reported.The participants were asked to answer questionnaires aimed at analyzing behaviors and psychopathology associated with eating disorders. The questionnaire focused on aspects such as participants’ dietary restraints and any concerns they had about weight, shape, and eating. Also, eating disorder behaviors, like binge eating, compulsive exercise, and laxative use were noted in participants.“Among all groups (men, women, and transgender individuals), any engagement in IF in the past 12 months was associated with greater eating disorder attitudes and behaviors,” Ganson explained. “Additionally, among women, in particular, IF was associated with all eating disorder behaviors, including binge eating, vomiting, laxative use, and compulsive exercise, while among men, IF was associated with compulsive exercising,” Ganson added.This study foreshadows, “IF may be problematic and associated with severe and harmful eating disorder attitudes and behaviors,” Ganson said, and added that “healthcare professionals need to be aware of these potentially correlated behaviors, as well as understand contemporary dietary trends like IF that are commonly discussed among young people, particularly on social media.”
Northeast Hospital Corporation, which operates facilities across Massachusetts, has agreed to pay $1.9 million in civil penalties to resolve allegations that it failed to keep accurate records of controlled substances.
The case emerged when Northeast discovered in 2018 that an employee had stolen more than 17,000 units of controlled substances.
“The settlement resolves allegations that Northeast’s recordkeeping was not in compliance with the CSA [Controlled Substances Act] and its regulations,” the U.S. Attorney’s Office for the District of Massachusetts said in a press release on Monday.
Northeast Hospital Corporation, part of Beth Israel Lahey Health, does business as Beverly Hospital in Beverly, MA, Lahey Outpatient Center Danvers in Danvers, MA, BayRidge Hospital in Lynn, MA, and Addison Gilbert Hospital in Gloucester, MA. Each location is separately registered with the Drug Enforcement Administration (DEA) to handle controlled substances.
According to the U.S. attorney’s office, the DEA began investigating Northeast after the hospital corporation reported in March 2018 that an employee had stolen 17,846 dosage units of controlled substances. The substances included fentanyl, Percocet, oxycodone, dextroamphetamine and MS Contin, a pain medication. The theft occurred over a period of more than a year.
Northeast was in the process of improving its pharmacy operations and controlled substances programs when it discovered the employee had stolen the drugs, according to the news release.
The DEA found that Northeast did not have an adequate record of each hospital’s inventory, which violates the CSA. Northeast also failed to report when controlled substances, including opioids, were transferred between hospitals, according to the press release.
“The CSA requires accurate inventorying and tracking of each controlled substance in circulation, from the manufacturer to the ultimate user,” the U.S. attorney’s office said.
For example, Northeast ordered controlled substances under Beverly Hospital’s DEA registration but then transferred those drugs to other Northeast locations without notifying the DEA.
“The recordkeeping requirements are intended, in part, to prevent misuse of controlled substances and avoid overdoses or other harms,” the U.S. attorney’s office said.
Northeast said it has implemented safeguards to prevent this from happening again.
“We are committed to ensuring the strongest possible safeguards for the handling of controlled substances and have robust policies and procedures in place, including anti-diversion software and strong audit and monitoring practices,” a spokesperson for Northeast Hospital Corporation said in an emailed statement.
Photo: Stuart Ritchie, Getty Images
Small molecules are a mainstay of drug therapy, many of them working by targeting a protein and blocking it. A newer but still experimental approach leads to the degradation of disease-causing proteins. Research has revealed new insights into the ways proteins can be regulated and Entact Bio is building on that science to expand what drugs can do. Rather than inhibiting or degrading proteins, the biotech startup aims to enhance them. Entact formally launched on Tuesday with $81 million to support its work in this new class of medicines.
To understand how Watertown, Massachusetts-based Entact aims to enhance proteins, it might help by starting with the mechanism that degrades them. An emerging field of drug research leverages a cellular disposal system whose role in degrading proteins is part of normal protein turnover in the body. Old or damaged proteins are marked for disposal with a molecular tag called ubiquitin. Therapies that harness this mechanism are small molecules that recruit ubiquitin to a disease-causing protein, which in turn gets it to go to the cellular trash bin.
Companies developing targeted protein degradation drugs have reached the clinic in oncology and inflammation. This science paved the way for what Entact CEO Victoria Richon calls “matchmaker molecules.” Protein degrader drugs, which are called proteolysis targeting chimeras, or PROTACs, bring together ubiquitin and a target protein. Entact calls its drugs enhancement-targeting chimeric medicines, or ENTACs. These molecules remove ubiquitin tags from proteins, sparing them from the cell’s disposal system.
“We’re actually enhancing protein function, so we’re actually doing the exact opposite [of PROTACs],” Richon said. “This expands our way of looking at different proteins we know are involved in disease.”
Entact’s proprietary technology, called Encompass, identifies proteins that are regulated by ubiquitin and associated with a disease. The platform then matches those proteins to a deubiquitinase, or DUB, an enzyme that can remove the molecular tag from a particular protein. Entact is not yet disclosing specific protein targets or therapeutic indications. But speaking generally, Richon said keeping key proteins out of the cellular trash bin could offer a new way to treat haploinsufficiencies, genetic disorders in which dysfunction of one gene of a gene pair leads to insufficient levels of a key protein. Cancer is another potential application. Some proteins function as tumor suppressors. Enhancing the activity of these proteins could offer a new way to fight cancer, Richon said.
Increasing levels of key proteins is just one way Entact aims to treat disease. Some diseases arise when proteins are in the wrong location in cells. Rather than completely removing ubiquitin, Richon said DUBs can also selectively shorten the molecular chain, which in turn changes where in the cell the protein goes. Shortening ubiquitin can also change a protein’s interaction with components of a cell or enhance its activity.
Entact is joining a small but growing group of drug developers working with DUBS. Versant Ventures-backed Stablix Therapeutics launched last year. The New York-based startup is based on Columbia University research that studied ubiquitin removal in cystic fibrosis. That initial research was published two years ago in Nature Methods. Vicinitas Therapeutics launched this past summer, the product of a research partnership between Novartis and the University of California, Berkeley. Early this year, the Berkeley scientists published research in in Nature Chemical Biology showing how they were able to stabilize protein levels in cystic fibrosis and cancer fibrosis.
Entact’s founders hold positions at places such as the Dana-Farber Cancer Institute, Harvard Medical School, University of Liverpool, and the Walter and Eliza Hall Institute of Medical Research. Richon, who was most recently the CEO of Ribon Therapeutics and is also a Sanofi veteran, said Entact’s technology is not licensed from a particular institution and the company holds its own patents for Encompass. She added that Entact is too early in its development to have published research, but the company’s scientific founders have published research about deubiquitinating enzymes.
Though Entact announced its latest financing on Tuesday, the Series A round is not new money. The financing closed last fall. Entact started in 2019. Seed financing supported research that showed the company’s approach could modify protein function, Richon said. With that proof-of-concept research in hand, Entact was able to raise the $81 million Series A round.
The company held off on unveiling its science and financing until now, which Richon said is a good time because of the progress Entact has made and the plans to add to its 10-person headcount. Entact is preclinical but Richon declined to go into further detail about the stage of Entact’s research, nor would she offer an estimate for when the research could reach clinical testing. Richon did say that the capital enables the startup to work on multiple programs at the same time.
The Series A round was co-led by Qiming Venture Partners USA and venBio Partners. New investors that joined the latest financing include Abingworth, Brandon Capital, Janus Henderson Investors, Logos Capital, Surveyor Capital, and Walter and Eliza Hall Institute of Medical Research, along with founding investors 4BIO Capital and Arkin Bio Ventures.
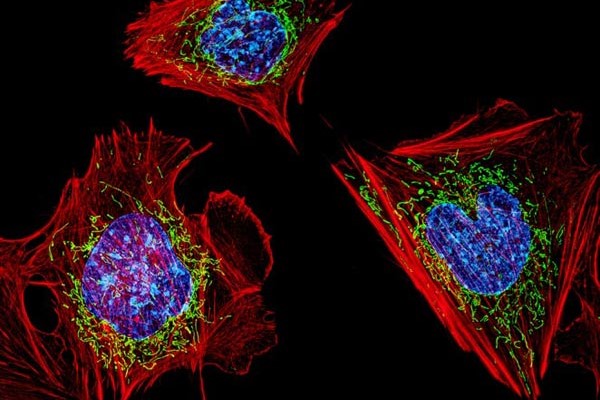
Public domain image by Flickr user NIH Image Gallery
About 40% of employed adults suffer from moderate to severe depression and/or anxiety, a new report found. The statistic is in stark contrast to national averages, which show that 11.4% of all adults experience depression and 8.2% suffer from anxiety.
The report was commissioned by Bengaluru, India-based Wysa, a company that created an AI chatbot for mental health support. Its app is available for consumers, employers, public health agencies, payers and providers. The startup chose to conduct the study after seeing the toll Covid-19 took on mental health, said Ramakant Vempati, co-founder and president.
“There’s this question mark: Is this behind us? Was this a blip? Is it back to normal? Are we going to go ahead and just carry on as before? Or is this something that has fundamentally changed?” Vempati said in an interview.
The mental health crisis is most certainly not behind working adults, the survey of 2,024 respondents in the U.S. and U.K. found. And management seems largely unaware of the issue. More than four in 10 workers said they suffer from anxiety, but their bosses don’t know. Another 38% said they suffer from depression that their employer isn’t aware of.
Many are afraid to say they need time off for mental health. About one in three employees tell their employers that they are physically ill in order to get a much-needed break and one in four use their vacation days. Another 42% just power through work without taking a break.
“There is openness to talking about it [now]. Even then, people feel hesitant in coming forward,” Vempati said. “I thought that was a very big, stark reminder of the challenge we have and how important it is to create mechanisms for people to get help without friction.”
When asked if they would prefer to talk about their mental health with an app — like Wysa — or someone from their workplace, most chose an app. Nearly 75% of respondents selected an app over human resources, 59% chose an app over their manager and 58% chose an app over a coworker. Even more shocking to Vempati is that 68% chose an app over a physician, although 55% selected a therapist over an app. These findings highlight the importance of digital mental health solutions in easing people’s stress, he added.
“That is reassuring, I think, to an employer who’s considering whether this is worth doing, or if this is going to actually move the needle,” Vempati said.
It’s not immediately clear whether other studies have been done that show people prefer an app over physicians, but the anonymity factor does play into privacy preferences generally when it comes to seeking mental health help.
Younger generations report higher levels of mental health struggles, the survey found. About half of working adults aged 16 to 34 suffer from moderate to severe depression, compared to one-third of those nearing retirement age. This could be that younger generations are more educated on mental health and are able to notice the signs better, or that older adults are more comfortable in their jobs after gaining more experience.
While mental health has become a priority for employers in recent years, the report is a reminder that more needs to be done, Vempati said. Employers need to make it easier for employees to access therapists. However, there are also cases when a therapist might not be the right solution, like for those experiencing financial distress or those in need of caregiving assistance. Employers need to provide support for those kinds of issues as well, Vempati said.
“The report is highlighting the fact that, number one, we are in a crisis,” he said. “We have a very large problem. Number two, it’s not going to go away. And number three, what we have right now is helping but we need to do more. We need to do much, much more.”
As healthcare costs rise for employers and the world experiences economic headwinds, Vempati stressed the importance of providing mental health support to employees, not cutting back.
“If you don’t intervene in mental health, you will have to pay in other ways because of churn, because of absenteeism, because of presenteeism and because of downstream medical costs,” he said. Presenteeism refers to when employees are not fully functioning while at work.
Photo: metamorworks, Getty Images